What You Need To Know
The aim of treatment is to prevent the development of osteoporosis and to prevent further bone loss in order to decrease the risk of osteoporotic fracture. Today there is a wide range of therapeutic options and several safe and effective pharmacological treatments that have been shown to act quickly (within one year) and to reduce the risk of fracture by up to 50%. It is important that the choice of treatment be tailored to a patient's specific medical needs and lifestyle.
Osteoporosis can be managed and treated by physicians from various areas of specialization; including general practitioners, endocrinologists, gynaecologists, rheumatologists, and orthopaedic surgeons. Osteoporosis patient and medical societies may be able to provide further information about physicians with special expertise in treating osteoporosis.
Treatment Modalities
- Risk Factor Reduction
- Nutritional Recommendations
- Pharmacological Therapies
- Surgical Treatment
- Miscellaneous Including Exercise And Psychological and Practical Support
Risk Factor Reduction
- Medications like steroids , thyroid hormone replacement under supervision
- Cessation of smoking and alcohol intake
- Eye-sight correction
- Hip protectors
- To avoid exposed wires, slippery rugs, loose carpets etc.
Nutritional Recommendations Calcium Optimal calcium intake reduces bone loss and suppresses bone turnover Adequate Calcium Intake.
| Life Stage Group | Estimated Adequate Daily Calcium Intake, mg/d |
| Young children (1–3 years) | 500 |
| Older children (4–8 years) | 800 |
| Adolescents and young adults (9–18 years) | 1300 |
| Men and women (19–50 years) | 1000 |
| Men and women (51 and older) | 1200 |
Vitamin D
The Institute of Medicine recommends daily intakes of 200 IU for adults 70 years.The daily dose of vit. D should be 400 IU along with calcium.
Other Nutrients:
1. Vitamin K is required for optimal bone mass
2. Magnesium and other dietary phytoestrogen
Pharmacological Therapies (Usually of two types )
Antiresorptive drugs : These are already available; slow the progressive thinning of bone.
Bone-building agents: These drugs help to rebuild the skeleton and are now becoming available or are in the developmental pipeline.
Antiresorptive drugs
Bisphosphonates
Bisphosphonates inhibit bone resorption. They are currently the first choice of treatment in a variety of bone metabolism disorders characterised by high bone resorption. They bring about an increase in bone mass and a decrease in fracture incidence in osteoporosis. There are different types of bisphosphonates which differ widely in their efficacy, side effects and possible routes of administration, thus offering a flexible range of therapeutic options.
Alendronate has been extensively studied for the treatment of osteoporosis under randomized controlled clinical trial conditions. Alendronate increases BMD at all skeletal sites and reduces the incidence of fracture by around 50% in both hip and spine. A newer bisphosphonate, risedronate, has also been shown to increase bone mass in postmenopausal women, reduce the rate of vertebral and nonvertebral fractures and reduce the risk of hip fractures in elderly women with a low BMD. More bisphosphonates, such as ibandronate and zoledronate, are in the late clinical development stage, offering additional options with respect to therapeutic formulations and dosage regimens.
Estrogen Analogs
Selective estrogen receptor modulators (SERMS) mimic estrogens in some tissues and anti-estrogens in others, and ideally provide the bone-retaining effects of estrogen without its unwanted side effects. Currently, the only marketed SERM is raloxifene. Raloxifene prevents bone loss and is indicated for the prevention and treatment of vertebral fractures in postmenopausal women. The incidence of new spinal fractures is reduced by 30-50% according to dose and existence or not of vertebral fractures at baseline – so far, no significant reduction in nonvertebral fractures has been reported. Raloxifene lowers serum cholesterol, does not induce endometrium bleeding or proliferation, and markedly decreases the incidence of breast cancer in osteoporotic women. Other SERMs, such as bazedoxifene and lasofoxifene, are in the late stages of clinical development.
Tibolone
Tibolone is a synthetic analog of the gonadal steroids with combined estrogenic, progestogenic and androgenic properties. Its effects on bone density are comparable to those of hormone replacement therapy. Its efficacy on fracture risk has not yet been assessed.
Calcitonin
Intranasal or injectable calcitonin is an alternative to HRT or bisphosphonates. The results of a study show that salmon calcitonin nasal spray reduces the incidence of vertebral fractures by 25-35% at a daily dose of 200 IU. This is a smaller reduction than that achieved by bisphosphonates or raloxifene, but some patients may benefit from the analgesic effect intranasal calcitonin has on bone pain. Salmon calcitonin nasal spray is available in some countries for the treatment of patients with vertebral fractures.
Hormone Replacement Therapy (HRT)
As a result of new studies on large numbers of women, the role of HRT has recently been re-evaluated. Although HRT has been shown to have a beneficial effect on bone and is still an option for the treatment of menopausal symptoms, there are other more effective and non-hormonal therapies available for the treatment of osteoporosis.
Bone-forming drugs
Parathyroid Hormone (Teriparatide)
The bone-forming effects of parathyroid hormone (PTH) have been known to exist for more than 70 years. However, it is only in the last 5-10 years that data have emerged that provide consistent and encouraging results in animals and humans. A recent multinational study on postmenopausal women with prior vertebral fractures demonstrates that a synthetic fragment of PTH will be useful in the management of osteoporosis. The results showed that the risk of vertebral fracture was reduced by 70% within 18 months of treatment. Nonvertebral fracture risk was reduced by 50%. It is expected that a form of injectable PTH will be available in some countries in the near future.
Strontium Ranelate
Strontium ranelate is a compound that has been shown in animal models to decrease bone resorption and increase bone formation. Following positive effects in a phase II clinical study, phase III clinical studies of strontium ranelate are under way to determine its effect on fracture in women with osteoporosis.
Orthopaedic Management
- Plasters, Rest, Splints
- Open Reductions & Internal Fixations – Plates, Screws, Dynamic Hip Screw (DHS, DCS), Moss Miami, Spine Fixation, External Fixators, Pedicle Screws, Sometimes Joint Replacement.
- Kyphoplasty
- Vertebroplasty
- Specially Designed Implants For Better Purchase In a Weak Osteoporotic Bone
Surgical Treatment Options ( For Osteoporotic Fractures) Common Osteoporotic Fractures: Around –Wrist, Hip, Pelvis, Spine
- Fractures of Wrist
- Fractures of spine
- Fractures of hip
- Fractures of Shoulder
- Vertebroplasty
- Kyphoplasty
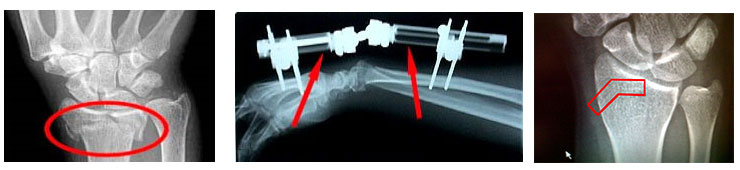
The common wrist fractures that occur are:
- Colles' fracture (distal radius)
- Smith's fracture (distal radius)
- Scaphoid fracture
- Barton's fracture (fracture dislocation of the radiocarpal joint)
- Chauffeur's fracture (fracture of the radial styloid)
- Greenstick fracture (confined to children)
- Fracture of the ulnar styloid
They also become more common with advancing age, partly because advancing age is related to an increased risk of falls and partly because of osteoporosis.
Patient will complain of severe pain, swelling and a visible deformity around the wrist region. There will be restriction of the normal range of movements of the wrist.
Treatment modalities include closed reduction and cast application to surgical treatment which includes diverse variety of implant application like pins, plates and external fixation.
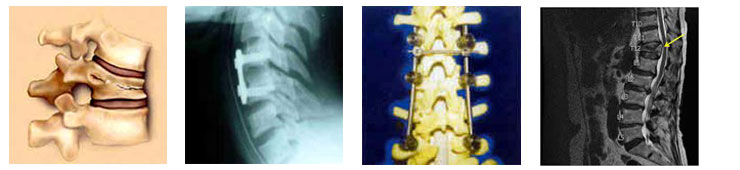
The main clinical symptoms of vertebral fractures (Osteoporotic spine involvement) typically include one or a combination of the following symptoms:
- Sudden onset of back pain
- Standing or walking will usually make the pain worse
- Lying on one’s back makes the pain less intense
- Limited spinal mobility
- Height loss
- Deformity and disability
Most patients diagnosed with a compression fracture in the spine describe the onset of pain immediately after a fairly routine activity that slightly strains or jars the back, such as:
Lifting - Opening a window or picking up a bag of groceries.
Bending - Picking something up off the floor.
Falling - jarring the spine by missing a step or slipping on ice.
For people with very advanced osteoporosis, the fracture can even occur with extremely minor activity, such as sneezing, coughing, getting in or out of the bathtub, or simply turning over in bed.
Treatment for the vertebral fracture will typically include non-surgical care, such as rest, pain medication and slow return to mobility, and/or surgical care, such as vertebroplasty or kyphoplasty, to help the fracture heal.
Measures to help prevent more vertebral fractures from occurring will typically include one or a combination of the following: calcium supplements, increased vitamin D, weight-bearing exercises, and hormone replacement therapy for women.

A hip fracture is a fracture in the proximal end of the femur (the long bone running through the thigh), near the hip joint.
The term "hip fracture" is commonly used to refer to four different fracture patterns and is often due to osteoporosis; in the vast majority of cases, a hip fracture is a fragility fracture due to a fall or minor trauma in someone with weakened osteoporotic bone.
The four common patterns found are:
- Femoral head fracture denotes a fracture involving the femoral head.
- Femoral neck fracture (sometimes Neck of Femur (NOF), subcapital, or intracapsular fracture) denotes a fracture adjacent to the femoral head in the neck between the head and the greater trochanter. These fractures have a propensity to damage the blood supply to the femoral head, potentially causing avascular necrosis.
- Intertrochanteric fracture denotes a break in which the fracture line is between the greater and lesser trochanter on the intertrochanteric line. It is the most common type of 'hip fracture' and prognosis for bony healing is generally good if the patient is otherwise healthy.
- Subtrochanteric fracture actually involves the shaft of the femur immediately below the lesser trochanter and may extend down the shaft of the femur.
The classic clinical presentation of a hip fracture is an elderly patient who sustained a low-energy fall and now has pain and is unable to bear weight. On examination, the affected extremity is often shortened and externally rotated (Outwards).
Most hip fractures are treated by orthopedic surgery, which involves implanting an orthosis e.g. Hemi replacement arthroplasty, Total hip replacement etc.Other procedures include Fixation with plates and screws. Sometimes an Intramedullary Nail is also used.
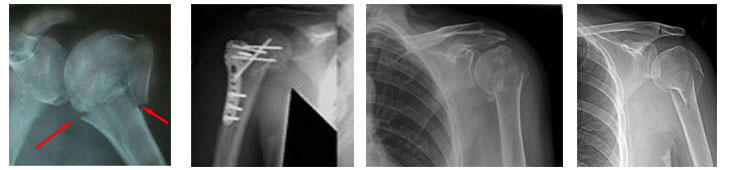
Proximal humerus fractures (Around shoulder) have been reported to account for about 5% of all fractures. These injuries usually occur in older patients who have osteoporotic, fragile bone. The fracture usually occurs from a ground-level fall. A much higher level of trauma would typically be required for a younger person to sustain the same type of fracture.
In general, 2- and 3-part fractures are treated with open reduction and internal fixation (a plate with screws is the choice of many surgeons currently). Four-part fractures in the younger, active patient also can be treated successfully with open reduction and internal fixation. However, in the elderly and in the patient with osteoporosis, a hemiarthroplasty is the treatment of choice.
Stiffness is the leading complication following non-operative or surgical treatment of a proximal humerus fracture
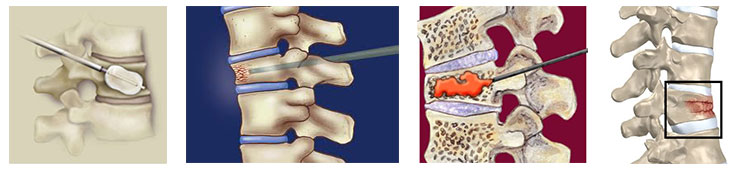
Vertebroplasty is a medical spinal procedure where bone cement is injected through a small hole in the skin (percutaneously) into a fractured vertebra with the goal of relieving the pain of osteoporotic compression fractures
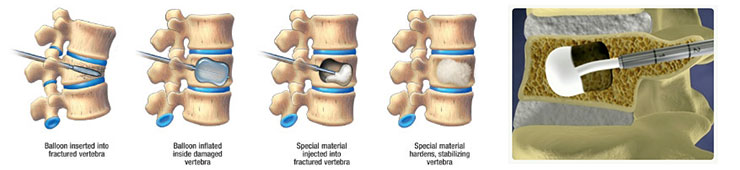
Kyphoplasty is a medical procedure that attempts to stop the pain caused by the bone fracture and attempts to restore the height and angle of kyphosis of a fractured vertebra (of certain types), followed by its stabilization using injected bone filler material.
yphoplasty and vertebroplasty represent the two procedures that percutaneously attempt to augment the strength of fractured or weakened vertebrae. 1. Specially Designed Implants For Better Purchase In a Weak Osteoporotic Bone
2. Plates, Screws, Dynamic Hip Screw (DHS, DCS), Moss Miami, Spine Fixation, External Fixators, Pedicle Screws, Sometimes Joint Replacement.
Exercise
Regular weight-bearing exercise has been shown to help maintain and build up bone mass. The stronger muscles, better balance and agility to which exercise contributes can also help in fall prevention. The type of exercise should be tailored to the individual's needs and abilities. People with osteoporosis must take special care when exercising to reduce the risk of fracture due to impact or falls.
Psychological and practical support
Rehabilitation following fractures, strategies for the prevention of falls, and psychological and practical support are important components of treatment. In addition to the practical help offered by many osteoporosis patient support groups, such groups can also be of great help in alleviating the feelings of isolation and depression experienced by many patients with severe osteoporosis.

